Protecting People With PPE
At the CDC’s Emergency Operations Center, Megan Casey ’04 offers guidance on finding and using personal protective equipment
June 5, 2020
By
Tina Eshleman
Megan L. Casey ’04 knows the importance of having the right personal protective equipment to guard against infection from a deadly virus.
As an Epidemic Intelligence Service officer with the Centers for Disease Control and Prevention, she trained ambulance drivers and evaluated hospital and clinic infection control practices in Sierra Leone during the West African Ebola outbreak in 2014.

Now, her expertise is directed toward health care workers and others who are at risk from the coronavirus. Based in the National Personal Protective Technology Laboratory at the CDC's National Institute for Occupational Safety and Health (NIOSH) in Morgantown, West Virginia, she supervises staff that provide guidance on the use of personal protective equipment in health care and other work settings.
Since January, Casey has been deployed as part of the United States Public Health Service (USPHS) coronavirus response. She is working remotely with the CDC Emergency Operations Center in Atlanta to support its Worker Safety and Health team, which has been operating around the clock to answer questions from the public about PPE, offer advice and find solutions to the challenges presented by the COVID-19 pandemic.
Among those challenges are persistent shortages of personal protective equipment. According to a survey by The Washington Post, in early May, 66% health care workers still didn’t have enough of the tight-fitting, NIOSH-approved N95 respirator masks that filter out most airborne particles. More than four in 10 reported shortages of the less protective and looser-fitting surgical masks, the newspaper reported. Although limited information is available about how many health care professionals have been infected with COVID-19, more than 9,000 cases had been reported by early April, according to the CDC.
Known as Megan Peery when she attended William & Mary, Casey earned a bachelor of business administration degree (double-majoring in marketing and government), then received a master of public health at Ohio State University and a bachelor of nursing from the University of Pittsburgh. She is a nurse epidemiologist, certified infection preventionist and a lieutenant commander in the U.S. Public Health Service.
While at W&M, Casey was a founder of Health Outreach Peer Educators (HOPE), a group of students trained to provide the university community with in-depth and interactive educational programs on topics such as nutrition, fitness, body image, use of alcohol and other substances, mental health and sexual health, recalls Michelle B. Alexander, a former health educator at the Student Health Center.
“Megan had an uncanny ability to motivate and empower the group,” Alexander wrote in a 2013 letter of recommendation for Casey when she applied to the Epidemic Intelligence Service. “I found myself continually impressed with her ability to stay in tune to the needs of her peers and to explore new ways in which to meet those needs using the resources available to her.”
Currently an assistant professor of health science at Thomas Nelson Community College in Williamsburg, Alexander says she has remained in contact with Casey since her graduation.
“Her courage, tenacity and dedication to global public health was on full display through the Ebola response effort and through her work now,” Alexander says. “She truly represents W&M at its finest.”
Casey recently answered a few questions related to her work at the CDC in response to COVID-19 and her experience at William & Mary.

What is your day like?
Right now, we have been very busy answering technical questions about the use of personal protective equipment in health care settings during COVID-19 but also other work settings as well. We’ve also been involved in writing guidance on the use of PPE in work settings during COVID-19.
What kinds of PPE are you evaluating?
NIOSH's National Personal Protective Technology Laboratory is responsible for approving respirators used in U.S. workplaces. You may notice the “NIOSH” logo on N95 or other respirator masks used in occupational settings. This involves making sure that all respirator models used in occupational settings meet minimum construction, performance and respiratory protection standards. NPPTL also conducts laboratory and field research, standards development, interventions and conformity assessment activities and does work related to other types of PPE such as gloves, safety goggles and protective clothing. NIOSH does not approve or certify surgical masks or other PPE items such as gowns, gloves and face shields.
How lengthy a process is the evaluation?
NPPTL’s focus areas during the COVID-19 outbreak includes: (1) supporting existing NIOSH respirator approval holders to increase their ongoing production; (2) quickly evaluating new domestic respirator applications for approval; and (3) providing up-to-date PPE guidance. NIOSH is not waiving any approval requirements; however, we are expediting the review of domestic approval holders. We anticipate that the administrative review and testing aspect of the approval process for respirators can be completed within 14 days for new domestic approval holders.
How are you helping health care workers find and use PPE?
We have been fielding many questions from health care workers and providing guidance. In some cases, health care workers are utilizing PPE that they may not be used to using, such as reusable elastomeric respirators or powered air-purifying respirators (PAPRs). We provide them information on how to use this equipment safely and answer questions about whether their PPE is appropriate for the hazards they may face on the job.
What are the biggest challenges you and your team face right now?
There is a lot that we don’t know about COVID-19, and that remains a major challenge for everyone involved in the response to this virus. However, we continue to use the best available science we have and apply it to the PPE questions.
Is there a success story you can share?
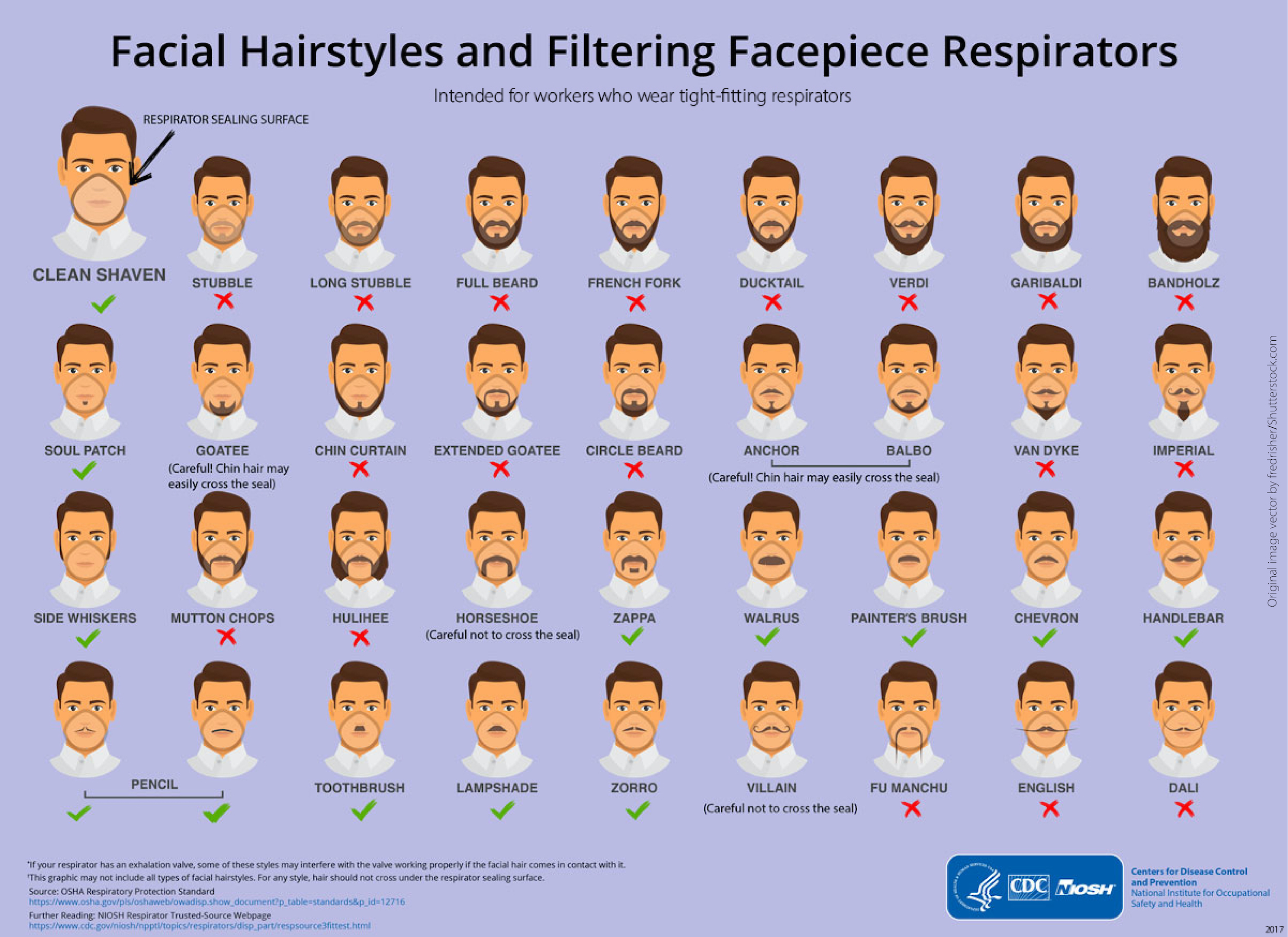
One of our infographics, “Facial Hairstyles and Filtering Facepiece Respirators,” was featured on CNN, “Good Morning America,” “The Late Show with Stephen Colbert” and many other programs. While it is humorous, we were very happy to hear people talking about how important it is to have a respirator mask that fits you correctly. I’m fortunate to supervise some very creative health communications staff members who developed this very popular infographic.
How do you anticipate your work will change in the coming weeks and months?
Pandemics and public health emergencies have a way of changing the way we understand public health and preparedness for these events. There may be increased interest in developing innovative PPE and research in preparation for large-scale events that require equipment to protect workers on the front lines.
How does your experience with COVID-19 differ from your experience with the Ebola virus?
While my experience with Ebola was in the field and my current work is in the CDC’s Emergency Operations Center, educating people on personal protective equipment and the correct use of PPE is very similar.
Why did you decide to go to William & Mary?
William and Mary has always promoted service above self, and I think that was one of the things that initially appealed to me. I’ve always been struck by how many of my W&M friends have found careers in public service.
Was anyone at W&M especially influential for you?
Professor Thomas Linneman’s Social Statistics class solidified my interest in survey research and epidemiology. Using social science to present statistical concepts was very easy for me to understand and really laid the groundwork for my future courses in biostatistics. He also played the best music during our statistical software labs. Professor Paul Manna was my thesis advisor, and he was wonderful at teaching me how to present information and data in a logical, cohesive way. Michelle Alexander at the Student Health Center was the first person who told me what epidemiology was and recognized that it was a good fit for me.
How did studying at William & Mary prepare you for your current role? What stands out to you about your time here?
I’ve used my marketing degree to help think about how to best communicate occupational health information and how to measure the impact of communication efforts. My undergraduate thesis was on infectious disease surveillance among county health departments. I also spent time doing peer health education with the Student Health Center. I spent a tremendous amount of time in nearly every single library at William & Mary, studying and writing. Being able to find a quiet spot among the books is one of my favorite memories. That, and all the brilliant friends that I made in those four years.